Nocturnal hypertension, or high blood pressure at night, is a significant health concern that often goes unnoticed. This condition is characterized by blood pressure readings of 120/70 mmHg or higher during the night.
Understanding Nocturnal Hypertension
In the USA, nocturnal hypertension is defined as nighttime blood pressure equal to or exceeding 120/70 mmHg. This condition can be further categorized into isolated nocturnal hypertension (INH). This is when high blood pressure is only observed at night, and combined daytime and nocturnal hypertension.
The prevalence of nocturnal hypertension varies among different populations. In a study involving 1344 individuals, 61.5% were found to have nocturnal hypertension. 12.9% had INH and 48.7% had combined daytime and nocturnal hypertension. Another study reported the prevalence of INH to be 22.8% in the general population. The concept of ‘dipping’ and ‘non-dipping’ blood pressure patterns is crucial to understanding nocturnal hypertension. Normally, blood pressure dips by 10-20% during sleep. This phenomenon is known as ‘nocturnal dipping’. However, in some individuals, this dip does not occur, leading to ‘non-dipping’ blood pressure patterns. Non-dipping patterns were observed in 32-46% of people with hypertension in one large study.
Risk Factors
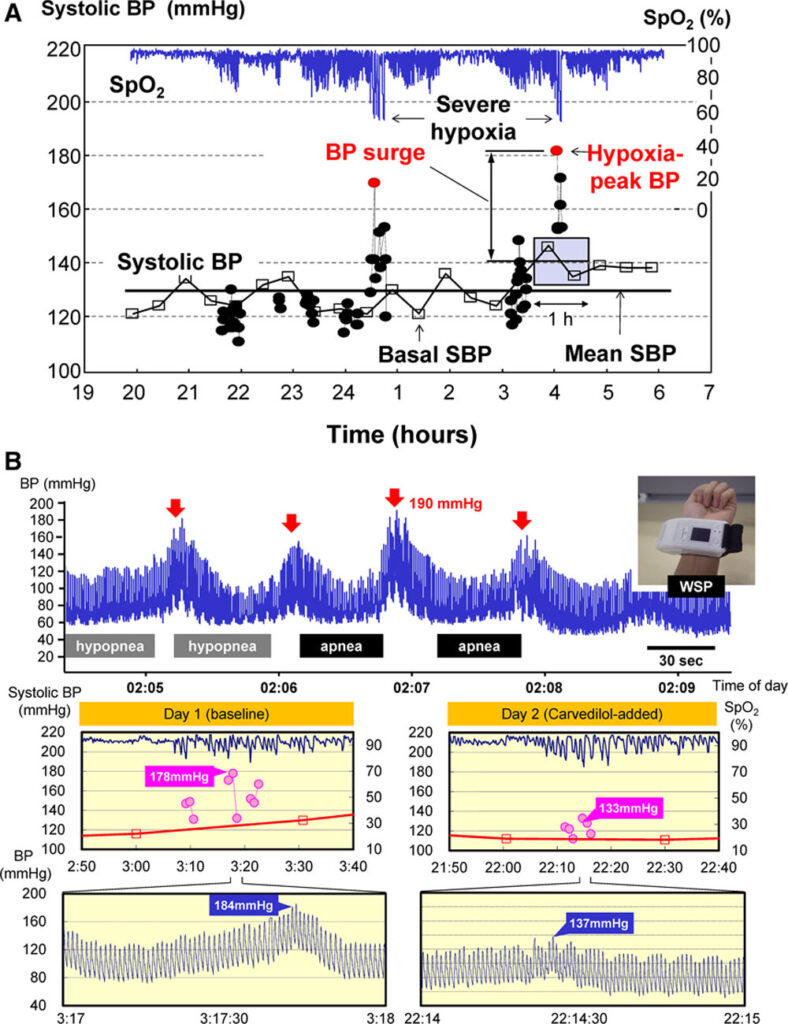
Several factors contribute to the development of nocturnal hypertension. These include increased sympathetic nervous system activity, hyperactivity of the renin-angiotensin-aldosterone system, sodium retention, and renal function impairment. Other potential risk factors include obstructive sleep apnea, diabetes, kidney disease, poor quality sleep, and lack of adequate sleep.
A study conducted in Buenos Aires reported that the prevalence of INH and masked nocturnal hypertension (MNH) varies. Researchers concluded that it is influenced by several factors. The list included diabetes, nighttime heart rate, sleep duration, older age, serum creatinine, and masked hypertension. The same study highlighted the high prevalence (49.7%) of isolated nocturnal masked uncontrolled hypertension (MUCH) in hypertensive patients with type 2 diabetes.
Management and Prevention
Effective management of nocturnal hypertension involves a combination of lifestyle modifications and pharmacological interventions. Lifestyle changes are the cornerstone of hypertension management and can significantly impact nighttime blood pressure levels.
- Sodium Restriction: Reducing salt intake can help lower blood pressure. The American Heart Association recommends no more than 2,300 milligrams (mg) a day for people with normal blood pressure. While no more than 1,500 mg per day for hypertension sufferers.
- Potassium Supplementation: Increasing dietary potassium through fruits and vegetables or supplements can counteract the effects of high sodium. It has been shown to lower blood pressure.
- Evening Medication: Some studies suggest that taking certain blood pressure medications at night can improve nighttime blood pressure control. For example, evening administration of blockers of the renin-angiotensin-aldosterone system has been shown to be effective.
- Melatonin Supplementation: Melatonin is a hormone that regulates sleep-wake cycles. It has been found to significantly reduce nocturnal systolic blood pressure when supplemented, indicating its potential as an adjunctive treatment.
Treatment Options and Innovations
Treatment for nocturnal hypertension may include the use of antihypertensive medications. They can be specifically timed to address nighttime blood pressure spikes.
- Bedtime Dosing of Antihypertensives: Some studies have found that taking blood pressure medications at bedtime can lead to better nighttime blood pressure control and reduce the risk of cardiovascular events.
- Melatonin Treatment: A specific treatment regimen involving 2 mg of melatonin taken nightly for 4 weeks significantly reduces nocturnal systolic blood pressure, suggesting its utility in treating nocturnal hypertension.
Innovations in treatment and monitoring
- Ambulatory Blood Pressure Monitoring (ABPM): ABPM is a method of measuring blood pressure over a 24-hour period, while the patient goes about their normal daily activities, including sleep. This tool has been instrumental in diagnosing nocturnal hypertension and assessing the effectiveness of treatments.
- Telemedicine and Digital Health: Advances in telemedicine and digital health technologies are enabling better patient monitoring and management of hypertension, including nocturnal hypertension. These technologies can provide patients and healthcare providers with real-time data and the ability to adjust treatment plans promptly.
Causes of Nighttime Blood Pressure Spikes
Nighttime blood pressure spikes, or nocturnal hypertension, can be caused by several factors:
- Sleep Apnea: This condition, characterized by repeated pauses in breathing during sleep, can lead to nocturnal hypertension.
- Kidney Disease: Impaired kidney function can lead to fluid retention and increased blood pressure, including at night.
- Diabetes: Diabetes can damage blood vessels and lead to increased blood pressure.
- High Salt Intake: Consuming too much salt can cause fluid retention and increase blood pressure.
- Stress: Chronic stress can lead to long-term increases in blood pressure, including at night.
- Lack of Adequate Sleep: Not getting enough sleep can disrupt the body’s natural circadian rhythm and lead to increased blood pressure.
- Sedentary Lifestyle: Lack of physical activity can contribute to high blood pressure.
Prevention and Management of Nighttime Blood Pressure Spikes
Preventing and managing nighttime blood pressure spikes involves both lifestyle modifications and medical interventions:
- Lifestyle Modifications: These include reducing salt intake, engaging in regular physical activity, managing stress through techniques like meditation or yoga, and ensuring adequate sleep.
- Dietary Changes: Avoiding excessive sodium in meals and choosing low-sodium alternatives can help control blood pressure.
- Evening Medication: Taking certain blood pressure medications at night can improve nighttime blood pressure control.
- Treatment of Underlying Conditions: Managing conditions like sleep apnea, diabetes, and kidney disease can help control nocturnal hypertension.
- Regular Monitoring: Regular blood pressure checks, including at night, can help detect and manage nocturnal hypertension.
What to Do When Nighttime Blood Pressure Spikes Occur
When nighttime blood pressure spikes occur, it’s important to:
- Consult a Healthcare Provider: If you experience symptoms of high blood pressure at night, such as frequent urination, difficulty breathing, or disrupted sleep, consult a healthcare provider.
- Adjust Medication Timings: If you’re already on blood pressure medication, your healthcare provider may recommend adjusting the timing of your medication to better control nighttime blood pressure.
- Manage Underlying Conditions: If you have conditions like sleep apnea, diabetes, or kidney disease, managing these conditions can help control nocturnal hypertension.
Prevalence of Nighttime Blood Pressure Spikes
Nighttime blood pressure spikes are quite common. In a study involving 5,292 untreated patients with hypertension, nighttime blood pressure was found to be a stronger predictor of cardiovascular outcomes than daytime blood pressure. Another study found that 99.2% of patients with masked uncontrolled hypertension had evidence of elevated nighttime blood pressures.