Does weight loss decrease blood pressure? Here is the new study to confirm it. Weight loss medication decreased both day and nighttime blood pressure readings, finds new study in the journal Hypertension.
Tirzepatide is a new medication for weight loss. It effectively reduced systolic blood pressure in around 500 obese adults after 36 weeks of use. The findings were featured in the American Heart Association‘s Hypertension journal. They indicate a decrease in systolic blood pressure by 7.4 mm Hg for the 5 mg dose, 10.6 mm Hg for the 10 mg dose, and 8.0 mm Hg for the 15 mg dose, with reductions observed during both day and night. This systolic measure of blood pressure is known as the top number in the readings. It is identified by the American Heart Association as a more accurate indicator of cardiovascular mortality risk than the diastolic (lower) number.
How does weight loss decrease blood pressure? Tirzepatide functions by simulating two metabolic hormones. It serves as an agonist for both the glucagon-like peptide-1 (GLP-1) receptor and the glucose-dependent insulinotropic polypeptide (GIP) receptor. These hormones enhance insulin release and its effectiveness post-meal, aiding in blood sugar regulation, slowing digestion, and suppressing appetite. This process results in a feeling of fullness, reduced food intake, and subsequent weight loss. In comparison, semaglutide only mimics the GLP-1 hormone and lacks GIP receptor agonism.
In 2022, tirzepatide received FDA approval for treating Type 2 diabetes. The following year, it was also sanctioned for chronic weight management in individuals with obesity (BMI ≥ 30 kg/m^2). It was also sanctioned for those with overweight (BMI of 27-29 kg/m^2). However, only those !!! have at least one weight-related health issue, like high blood pressure, Type 2 diabetes, or high cholesterol.
“Our findings indicate treating obesity with the weight loss medication tirzepatide may be an effective strategy for preventing or treating high blood pressure,” said lead study author Professor James A. de Lemos, M.D., Chair of cardiology at UT Southwestern Medical Center in Dallas. “Although tirzepatide has been studied as a weight loss medication, the blood pressure reduction in our patients in this study was impressive. While it is not known if the impact on blood pressure was due to the medication or the participants’ weight loss, the lower blood pressure measures seen with tirzepatide rivaled what is seen for many hypertension medications.”
How does weight loss decrease blood pressure? Study background and details
SURMOUNT-1 was a randomized study on the effect of increasing doses of tirzepatide on weight loss. It found that in participants with overweight or obesity (body mass index (BMI) ≥27 kg/m2), once-weekly injections of 5 mg, 10 mg or 15 mg of tirzepatide led to mean weight reductions of 15%, 19.5% and 20.9%, respectively, compared to placebo.
The sub-study included 600 adults from SURMOUNT-1: 155 participants received placebo; 145 were taking tirzepatide 5 mg; 152 were taking tirzepatide 10 mg; and 148 were taking tirzepatide 15 mg.
Blood pressure measurements were available and analyzed for 494 participants who valid ambulatory blood pressure monitoring data at the beginning of the study and at week 36.
Only the study participants with at least 70% valid readings on ambulatory monitoring and a minimum of 20 daytime and seven nighttime readings were included in the data analyses. This was 494 out of 600 initial participants.
69% of study participants self-identified as female, and 31% self-identified as male. 66.8% self-identified as white adults, 11.8% self-identified as Black adults and 25% self-identified as Hispanic ethnicity.
The average age of the participants was 45.5 years, and their average BMI was 37.4 kg/m2, which meets the criteria for obesity (obesity is BMI≥30). People with obesity have an increased risk of high blood pressure, heart disease, stroke and Type 2 diabetes, as well as other health conditions.
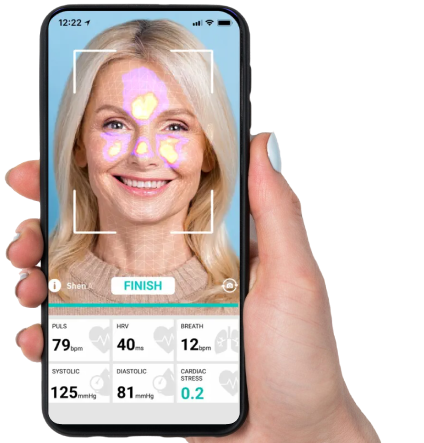
Ambulatory blood pressure monitoring used in this study included blood pressure measurements every 30 minutes during the day and every hour at night, providing a more comprehensive assessment of blood pressure than in office or daily home blood pressure measurements. For ambulatory blood pressure monitoring, study participants wore a blood pressure monitoring device for a 24- to 27-hour period that measured blood pressure throughout waking and sleeping hours. Ambulatory blood pressure monitoring was conducted when participants first began taking tirzepatide at the start of the study and after 36 weeks of being enrolled in the study.