I am so happy to introduce the readers of this blog to the man in the center of innovations at the world’s largest and one of the oldest organizations in heart health, the American Heart Association. Many of you know the AHA’s heart.org, the leading online content source of credible information on blood pressure. Currently, the American Heart Association has over 35 million volunteers and supporters. The AHA itself supports over 1,700 cardiovascular and cerebrovascular research projects, and is the frontrunner in technological advances of blood pressure monitoring. Please meet Dr. Patrick Dunn, the Program Director of the American Heart Association Center for Health Technology and Innovations.
The AHA CHT&I activities
Dr. Dunn, if you were to describe the activities of the AHA Center for Health Technology and Innovations to a hypertension patient, how would you do it?
Dr. Patrick Dunn: Our role is to connect with technology solutions that align with AHA science. Blood pressure is a key factor in understanding ideal cardiovascular health and managing acute and chronic health conditions. Unlike many healthcare diagnostics and biomarkers, patients have many opportunities to get blood pressure readings, including home blood pressure monitors, wellness and fitness centers, and kiosks in employer and retail centers.
A key role for Center for Health Technology and Innovation is helping patients (and front line healthcare professionals) understand the importance of getting a valid blood pressure reading and getting information from a trusted source. Health technology solutions can access content and care plans from our API enabled content management system.
Finally, we help health technology solutions provide a higher level of evidence that their solution is moving the needle in the right direction.
Future of blood pressure monitoring
In our talk prior to this interview, you mentioned that the AHA Center for Health Technology and Innovation ‘tries to stay a bit ahead’ with regards to the technological advancements in blood pressure monitoring. What is likely to come? Perhaps, you could elaborate on the near (1-3 years) and mid term (3-5 years) future?
Dr. Patrick Dunn: The American Heart Association is celebrating its 100 year anniversary this year and we are the organization, along with the American College of Cardiology that establishes the guidelines for prevention, detection, awareness, management, and control of hypertension. Our guidelines, scientific statements and policy statements must be science and evidence based, using the highest level of evidence.
The Center for Health Technology and Innovation was formed in 2016 as a center of excellence for technology and innovation. We are a connector between the technology world and the clinical and scientific communities. Our role is to help the tech world better understand the science, and it is to help the clinical world understand how to use the technology. That places us at the intersection of technology and innovation.
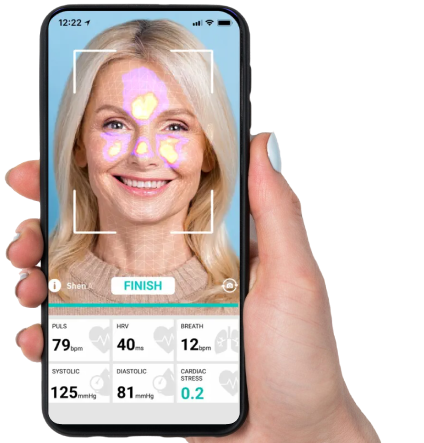
Part of our role is to help the AHA see what is coming and be able to respond. In the case of blood pressure monitoring, the next big thing will be ‘cuffless’ blood pressure monitoring. While the AHA still recommends having a blood pressure taken in the upper arm, with an arterial occlusion method, non-invasive, non-occlusive methods keep getting better. While these methods might not be ready to change the guidelines in the near term, they can still play a role by improving access to blood pressure readings, and in the long-term will likely change how blood pressure is monitored and treated.
Continuous monitoring
Many innovative technologies claim to ensure continuous monitoring. What are the benefits and downsides, if any, of the continuous blood pressure monitoring? What is the AHA’s approach to such technologies?
Dr. Patrick Dunn: The benefits of continuous blood pressure monitoring is that you can see blood pressure trends throughout the day in response to activities. If you think about it, life and death decisions on how to treat blood pressure are based on 2 numbers (systolic and diastolic), taken a couple of times per year, in an unnatural setting (in a stationary, resting setting).
Continuous readings would allow blood pressure to be treated in a similar way to how diabetes is treated. Patients and healthcare professionals can see trends throughout the day, and even while sleeping. Patients can be alerted if the blood pressure is too high or too low and deploy countermeasures.
The downside is what do we do with all of this information. How would a physician be able to manage the flow of information? The role of the AHA is to focus on ensuring that the readings are valid and the level of evidence is high enough to make treatment and policy decisions. In the long run the AHA could help determine how the information is used in an evidence-based manner.
AI in blood pressure
There are reports about the research on employment ML algorithms on population level blood pressure datasets to develop tools that aim to identify patterns, predict spikes and even predict blood pressure readings. Where are we now in this development, what challenges are to be addressed, in your opinion?
Dr. Patrick Dunn: What does the future of AI and ML in healthcare look like? If we can harness the power of AI, like we have with disease, the genome, and the atom, then we have the potential to create a more equitable healthcare system. Reducing the administrative burden imposed on healthcare professionals may allow them to spend more time in actual patient care. Patterns can be identified leading to earlier identification of health conditions and more personalized plans of care.
Regardless of the form of AI, the best practice is to consider AI/ML an assistant and subordinate to human thinking and decision making. Human enabled AI can allow highly trained professionals to focus on care and critical decision making rather than having to focus on repetitive tasks, such as documentation of the encounter in the electronic health record. Ultimately, more research is needed, and more conversation and better documentation of the pros and cons of AI are necessary.
The challenges with using AI/ML include (1) bias in AI, (2) the risks that the system is ‘hallucinating’ (making things up), and (3) lack of transparency. While these are concerns, these are also very human traits that we should always be concerned about, with or without AI/ML.
Digital health for hypertension
Hypertension affects up to half of the US population. What formats of digital health solutions, in your view, can contribute best to blood pressure awareness and hypertension management?
Dr. Patrick Dunn: The American Heart Association has emphasized the need to reach patients in ways that will lead to successful and sustainable behavioral changes. After decades of steady improvement in the awareness, treatment, and control of hypertension in the United States, there has been a troubling decline in blood pressure control. These numbers have been exacerbated by the pandemic and indicate even wider disparities when social determinants of health are considered.
There is no shortage of conditions that can benefit from the use of technology, including high blood pressure, heart attack and heart failure, stroke and post-stroke rehab, atrial fibrillation, peripheral artery disease, cardiac rehab and secondary prevention, and the metabolic syndrome. There also is a range of technologies that can be used to prevent, support and/or manage these conditions, including mhealth/digital health medication adherence, behavior change and coaching, telemedicine, AI, EMR based interventions, and many others.
Wearable and implanted devices have been shown to predict abnormal heart rhythms, such as atrial fibrillation, while connected devices have been used to manage diabetes and hypertension. Digital health interactions can be clinician to patient, clinician to clinician, in synchronous and asynchronous or mixed modes and have been used for risk factor monitoring, medication adherence, and symptom monitoring.