New research suggests that in vitro fertilization with frozen embryos can substantially increase a woman’s risk of high blood pressure complications during pregnancy.
According to a study published in the American Heart Association journal Hypertension, fertilization with frozen embryos increases the risk of pregnancy complications caused by high blood pressure by 74% compared to fertilization with fresh embryos or natural conception.
‘Some doctors have begun skipping fresh embryo transfer to routinely freeze all embryos’
Dr. Sindre H. Petersen, Norwegian University of Science and Technology
Researchers concluded that the higher risk was associated with the in vitro fertilization process, not with the parents, after comparing siblings born with fresh and frozen embryos.
“Frozen embryo transfers are now increasingly common all over the world, and in the last few years, some doctors have begun skipping fresh embryo transfer to routinely freeze all embryos in their clinical practice, the so-called ‘freeze-all’ approach,” lead study author Dr. Sindre H. Petersen, a PhD fellow at Norwegian University of Science and Technology.
The results demonstrate that all benefits and harms must be carefully considered before freezing all embryos routinely.
There are several disorders that can cause high blood pressure, or hypertension, during pregnancy, including preeclampsia. Preeclampsia occurs in roughly one in 25 pregnancies in the United States.
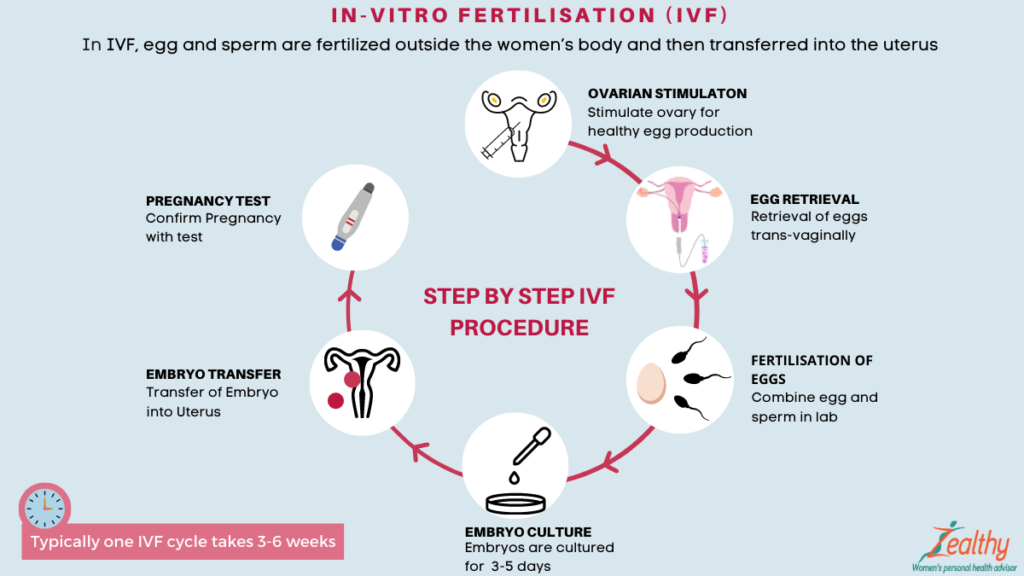
By using IVF (in vitro fertilization), eggs are removed from the mother’s ovaries and fertilized in the lab by sperm, resulting in an embryo. Cryopreservation can be used to freeze the fresh embryo or to transfer it to the mother’s uterus. After thawing, the frozen embryo can be transferred to the uterus. Due to recent advancements in cryopreservation technology, freezing embryos has become more common.
The use of frozen embryos has been associated with a higher risk of pregnancy complications related to high blood pressure, but researchers are not sure whether the risk stems from the freezing process or parental risk factors.
Researchers analyzed medical data for 2.4 million women in Denmark, Norway, and Sweden who gave birth between 1988 and 2015. They ranged in age from 20 to 44. There were 4.4 million naturally conceived pregnancies, 78,000 pregnancies resulting from fresh embryo transfers, and 18,000 pregnancies resulting from frozen embryo transfers in the study. Three thousand sibling comparisons were also included, in which siblings were conceived differently by the same mother.
When frozen embryos were used during IVF, the risk of hypertension during pregnancy increased by 74% compared to those who used fresh embryos.
Among women who conceived through frozen embryo transfer and natural conception, the risk of developing hypertensive disorders during pregnancy was twice as high.
“Our sibling comparisons indicate that the higher risk is not caused by factors related to the parents,” but rather that IVF treatment factors may be involved, Dr Petersen said.
Premature births were also found to be more common in babies conceived using IVF. The percentage of babies born before 40 weeks of gestation conceived using frozen embryos was 7%, while the percentage of babies born with fresh embryo transfers was 8% compared to 5% for those conceived naturally.
“Our results highlight that careful consideration of all benefits and potential risks is needed before freezing all embryos as a routine in clinical practice,” Dr Petersen said. “A comprehensive, individualized conversation between physicians and patients about the benefits and risks of a fresh versus frozen embryo transfer is key.”